Chronic venous insufficiency (CVI) is a common but often overlooked health issue that affects the proper flow of blood in the veins, primarily in the legs. If left untreated, CVI can lead to discomfort, skin changes, and more serious complications. In this article, we’ll break down everything you need to know about CVI—its causes, symptoms, and the treatment options available.
🧬 What Is Chronic Venous Insufficiency?
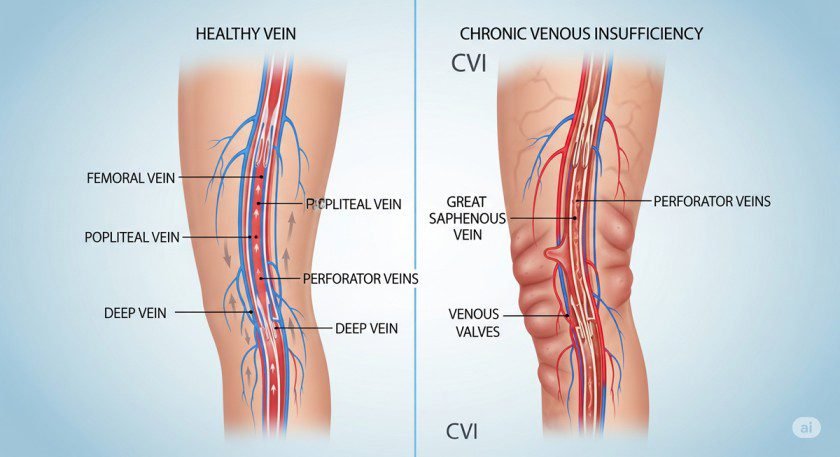
Chronic venous insufficiency is a condition where the veins in the legs are unable to return blood efficiently back to the heart. Normally, one-way valves in the veins prevent blood from flowing backward. In people with CVI, these valves become damaged or weak, causing blood to pool in the legs.
Over time, this can result in swelling, pain, and skin changes. While it’s not typically life-threatening, CVI can significantly affect your quality of life if not addressed.
⚠️ Causes of Chronic Venous Insufficiency
Several factors contribute to the development of CVI. Here are some of the most common causes:
- Prolonged Standing or Sitting: Jobs that require standing or sitting for long hours (like nurses, cashiers, or office workers) increase CVI risk.
- Obesity: Excess body weight puts added pressure on leg veins.
- Pregnancy: Hormonal changes and increased blood volume can strain the venous system.
- Aging: Veins and valves weaken with age.
- History of Deep Vein Thrombosis (DVT): Blood clots can damage vein valves.
- Genetics: A family history of varicose veins or vein disease increases your risk.
🩻 Symptoms of Chronic Venous Insufficiency
CVI symptoms often develop gradually. Pay attention to these signs:
- Swelling in the lower legs or ankles (especially after standing for long periods)
- Aching, cramping, or heaviness in the legs
- Itchy or flaky skin on the legs or feet
- Varicose veins or spider veins
- Darkening or discoloration of the skin
- Open sores or ulcers near the ankles
If you notice persistent leg discomfort or skin changes, it’s important to seek medical advice for a proper diagnosis.
🩹 Treatment Options for Chronic Venous Insufficiency
Fortunately, CVI can be managed effectively with a combination of lifestyle changes, medical treatments, and procedures. Here are the most common approaches:
1. 🧦 Compression Therapy
Wearing compression stockings is a non-invasive and effective way to improve blood flow and reduce swelling. These garments help squeeze the leg veins, pushing blood back toward the heart.
2. 🧘 Lifestyle Changes
Elevate your legs regularly to help blood circulation.
Exercise daily, especially walking, to strengthen calf muscles.
Avoid long periods of standing or sitting.
3. 💊 Medications
Doctors may prescribe medications to improve blood flow or treat underlying inflammation. In some cases, diuretics may be used to reduce swelling.
4. 🩻 Minimally Invasive Procedures
Sclerotherapy: Injects a solution into varicose veins to close them.
Endovenous laser therapy (EVLT): Uses laser energy to seal damaged veins.
Radiofrequency ablation (RFA): Similar to EVLT but uses radiofrequency waves.
5. 🏥 Surgical Treatment
In more severe cases, procedures like vein stripping or bypass surgery may be necessary. These are typically considered when less invasive treatments fail.
🛡️ Prevention Tips for CVI
Preventing chronic venous insufficiency is all about improving circulation and reducing pressure on your leg veins. Here are a few tips:
- Maintain a healthy weight
- Stay active and avoid sitting too long
- Wear compression socks if you’re at risk
- Avoid tight clothing around the waist and legs
- Elevate your legs while resting
🧾 Final Thoughts
Chronic venous insufficiency is more common than you might think—and it’s manageable. Recognizing the early signs, making lifestyle changes, and seeking the right treatment can dramatically improve your leg health and overall well-being.
If you or someone you know is experiencing the symptoms of CVI, consult a healthcare provider for proper evaluation and care.


